12 Mar | 2019
Spatial patterns of white matter hyperintensities are associated to Alzheimer’s disease risk factors
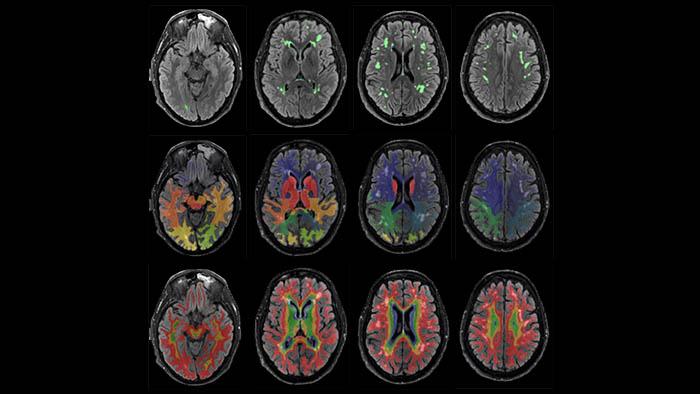
White matter hyperintensities
White matter hyperintensities are brain lesions of vascular origin that are associated with a higher risk of developing Alzheimer’s disease. Researchers from the Alzheimer’s Prevention Program at the Barcelonaβeta Brain Research Center (BBRC), who are also members of the CIBERFES and CIBER-BBN, have published in Alzheimer’s Research & Therapy a new study which reveals spatial patterns of white matter hyperintensities associated to risk factors of the disease.
The aim of the study was to describe the patterns of white matter hyperintensities associated with dementia risk estimates and individual risk factors in a cohort of cognitively unimpaired individuals aged from 51 to 64. Data was collected in 575 participants from the Alfa Study of the Pasqual Maragall Foundation and “la Caixa”.
White matter hyperintensities load was calculated from in each brain lobe and in four equidistant layers from the ventricular surface to the cortical interface. Global volumes and regional patterns of the load of these lesions were analyzed as a function of the Cardiovascular Risk Factors, Aging and Dementia (CAIDE) dementia risk score, as well as family history of the disease and Apolipoprotein E (APOE) genotype, as certain expressions of this gene are associated with a higher risk of dementia.
Age, hypertension, hypercholesterolemia and body mass index as risk factors
The results of the study showed that higher levels of dementia risk are associated with an increased global load of white matter hyperintensities. Age and hypertension were the main drivers of this association, while hypercholesterolemia and body mass displayed a minor, albeit significant influence.
Regionally, higher levels of dementia were associated with white matter hyperintensities in anterior areas, mostly in frontal lobe. Participants with maternal family history of the disease had a higher load of these lesions, especially in temporal and occipital lobes.
The study also revealed a protective effect of APOE-Ɛ2 over global white matter hyperintensities.
“The load of white matter hyperintensities is associated with Alzheimer’s disease risk factors even in subjects without cognitive impairment and with very low white matter hyperintensities burden and dementia risk estimates”, explains Dr José Luis Molinuevo, head of the Alzheimer’s Prevention Program at BBRC. According to the first author of the study, Gemma Salvadó, “our results suggest that tight control of modifiable risk factors in middle-aged individuals could have significant impact in reducing the risk of developing dementia in the future”.